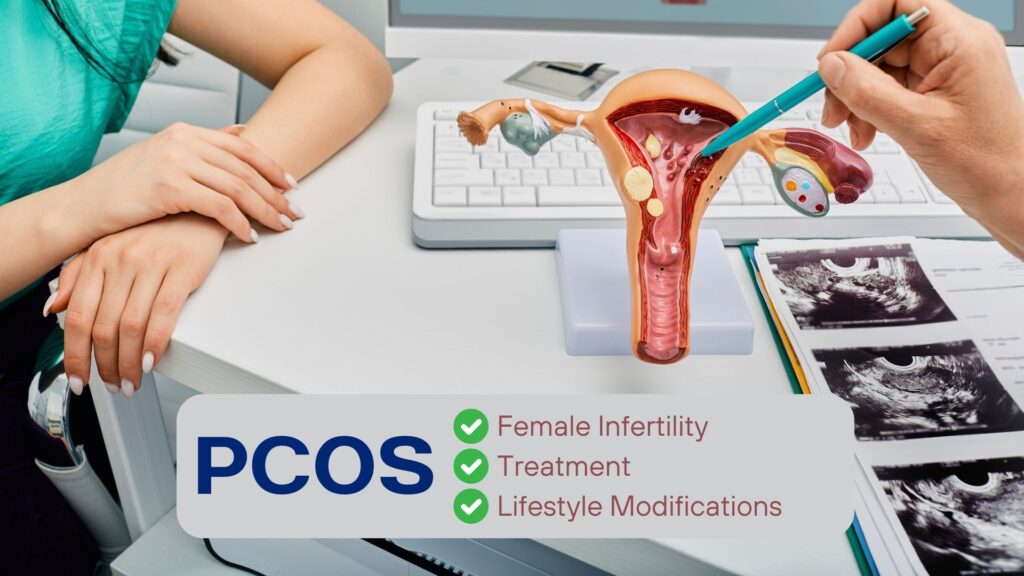
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It’s characterized by a combination of symptoms, including irregular menstrual cycles, hormonal imbalances (excess male sex hormone), and the presence of cysts on the ovaries. It’s called “polycystic” because the ovaries of women with PCOS may contain many small cysts, which are small fluid-filled sacs.
PCOS is highly prevalent, affecting approximately 1 in 10 women, making it one of the most common endocrine disorders among women. Importantly, PCOS significantly impacts women’s reproductive health and quality of life. It’s a leading cause of infertility in women, contributing to a substantial percentage of cases. Given its serious impact on reproductive health, understanding PCOS and its implications for fertility is essential. Beyond fertility, PCOS also affects various aspects of sexual health, such as menstrual irregularities and emotional well-being. Therefore, discussing PCOS within the context of sexual health is crucial for promoting overall reproductive well-being and addressing related concerns effectively.
PCOS & Infertility
Polycystic Ovary Syndrome (PCOS) significantly impacts fertility in women. One of the main reasons for infertility in PCOS is the irregular ovulation, reducing the chances of conception. Hormonal imbalances associated with PCOS, such as elevated levels of androgens (male hormones) and insulin resistance, can disrupt the normal process of ovulation. These hormonal disturbances can affect the development and release of eggs from the ovaries, making it difficult for women with PCOS to conceive. Additionally, hormonal imbalances associated with PCOS can manifest as symptoms such as acne, excessive hair growth (hirsutism), and weight gain
Additionally, the presence of ovarian cysts, although not always necessary for a diagnosis of PCOS, can contribute to fertility issues. These cysts may interfere with the normal functioning of the ovaries, further affecting the release of eggs and hormone production. Polycystic Ovary Syndrome (PCOS) can manifest in various forms, with two distinct types being Menorrhagia and Amenorrhea. These types present its own unique challenges and implications for women’s health and fertility.
Also Read: Painful Intercourse in Women – Reasons & Treatment
Menorrhagia
Menorrhagia is abnormally heavy, frequent or prolonged menstrual bleeding. Women experiencing menorrhagia often endure excessive bleeding during menstruation, leading to frequent changes of sanitary products and prolonged periods lasting longer than seven days. This condition increases the risk of anemia due to blood loss, resulting in symptoms such as fatigue, breathlessness and weakness. Additionally, unpredictable menstrual cycles pose challenges for fertility and reproductive health.
Amenorrhea
Amenorrhea on the other hand is the absence of menstrual periods. Women experiencing amenorrhea may not have menstrual periods for several months or longer, leading to difficulties in conception and infertility concerns. Prolonged amenorrhea can lead to a buildup of the uterine lining (endometrium), increasing endometrial thickness and also raising the risk of endometrial cancer if left untreated. Prolonged amenorrhea, can also lead to decreased estrogen levels, which may affect bone density and increase the risk of osteoporosis and bone fractures over time.
PCOS & Hormonal Imbalance
Polycystic Ovary Syndrome (PCOS) is often associated with insulin resistance, a condition in which cells throughout the body become less responsive to the effects of insulin. Insulin resistance plays a significant role in the pathophysiology of PCOS and contributes to various metabolic and reproductive abnormalities observed in affected individuals.
Insulin is a hormone produced by the pancreas that helps in the uptake of glucose into cells for energy production. In insulin-resistant individuals, cells become less responsive to the actions of insulin, leading to impaired glucose uptake and increased blood sugar levels. To compensate for this reduced sensitivity to insulin by the body, the pancreas secretes more insulin, resulting in hyperinsulinemia (elevated insulin levels in the bloodstream).
Increased insulin levels (hyperinsulinemia) can stimulate the ovaries (theca cells of ovaries) to produce excess male hormones (androgens), including testosterone. Additionally, high levels of insulin indirectly reduce the production of sex hormone-binding globulin (SHBG) in the liver, which binds to circulating testosterone, reducing its bioavailability. With lower levels of SHBG, more testosterone remains unbound and active in the bloodstream.
Additionally, increased insulin levels can also impair the balance of two other important hormones – luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which play a very important role in regulating periods in women. This imbalance of LH/FSH ratio disrupts normal ovarian function, inhibiting follicular development and ovulation.
Treatment for PCOS
Treatment for Polycystic Ovary Syndrome (PCOS) involves a multifaceted approach aimed at managing symptoms, restoring hormonal balance, and addressing underlying metabolic disturbances. The goals of treatment include improving menstrual regularity, promoting ovulation, reducing androgen levels, and addressing long-term health risks associated with PCOS, such as insulin resistance and cardiovascular disease.
Oral contraceptive pills (OCPs), containing estrogen and progestin, are commonly prescribed to regulate menstrual cycles, reduce androgen levels, and alleviate symptoms such as acne and hirsutism. Anti-androgen medications, such as spironolactone and finasteride, may be used to block the effects of androgens and mitigate excess hair growth and acne. Insulin-sensitizing agents, like metformin, are frequently utilized to improve insulin sensitivity and regulate menstrual cycles, particularly in individuals with insulin resistance. Ovulation-inducing medications, including clomiphene citrate and letrozole, are prescribed to stimulate ovulation in women with PCOS who are trying to conceive.
Lifestyle Modifications for PCOS
Lifestyle modifications are extremely important in managing Polycystic Ovary Syndrome (PCOS) as they directly address underlying metabolic dysfunctions and contribute to symptom alleviation. One crucial aspect is weight management, particularly significant for overweight or obese individuals with PCOS. Excess weight exacerbates insulin resistance and hormonal imbalances, worsening PCOS symptoms. Therefore, shedding even a modest percentage of body weight, around 5-10%, can lead to notable improvements in symptoms and reproductive outcomes.
A balanced diet is paramount for PCOS management, focusing on the composition of meals. Incorporating a mix of carbohydrates, proteins, and healthy fats is essential. Dietary fats, particularly monounsaturated and polyunsaturated fats found in sources like avocados, nuts, seeds, and olive oil, aid in improving insulin sensitivity and reducing inflammation. However, it’s vital to be mindful of portion sizes as fat is calorie-dense and may easily lead up to a calorie surplus diet and weight gain, if not mindful of the total calorie intake. It is also important to opt for healthier fat choices over saturated and trans fats, which can exacerbate insulin resistance and increase cardiovascular risks.
Regular physical activity is instrumental in combating insulin resistance and promoting weight loss, both of which are vital for individuals with PCOS. Both aerobic exercises, like jogging, or cycling, and resistance training, such as weightlifting or bodyweight exercises, are beneficial. Resistance training, especially, enhances muscle mass and improves insulin sensitivity. Engaging in at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity per week, alongside muscle-strengthening exercises on two or more days, is recommended.
Moreover, ensuring sufficient sleep and effective stress management are crucial for individuals with PCOS. Inadequate sleep quality and chronic stress can exacerbate insulin resistance and hormonal imbalances, worsening PCOS symptoms. Striving for 7-9 hours of quality sleep per night and integrating stress-reduction techniques such as mindfulness meditation, deep breathing exercises, or yoga into daily routines can significantly enhance overall well-being and support PCOS management efforts.
How can we help?
At SOLVE, we provide comprehensive support and guidance for individuals managing Polycystic Ovary Syndrome (PCOS) through our expert panels of doctors and lifestyle specialists. Our expert panels comprise gynaecologists and infertility specialists who specialize in the diagnosis and management of PCOS-related reproductive health issues. These specialists possess extensive knowledge and experience in treating PCOS, offering personalized care tailored to each individual’s unique needs. They are equipped to address various aspects of PCOS, including irregular menstrual cycles, ovulation problems, fertility concerns, and hormonal imbalances. Our gynecologists and infertility specialists work closely with patients to develop customized treatment plans aimed at optimizing reproductive outcomes and improving overall quality of life.
In addition to our medical experts, SOLVEMyHealth boasts an expert team of lifestyle specialists, including dietitians and exercise physiologists, who play a crucial role in supporting individuals with PCOS in adopting healthy lifestyle habits. Our diet and exercise specialists are well-versed in the dietary and lifestyle modifications necessary for managing PCOS, including weight management, balanced nutrition, regular physical activity, and stress management. They provide evidence-based guidance and practical strategies to help individuals with PCOS make sustainable lifestyle changes that promote better metabolic health, hormonal balance, and overall well-being.
Through our multidisciplinary approach, SOLVEMyHealth aims to empower individuals with PCOS with the knowledge, tools, and support they need to effectively manage their condition and improve their quality of life.