Painful intercourse, a complex and multifaceted phenomenon, presents a significant challenge for many women, affecting both their physical comfort and emotional well-being. At its core, the experience of pain during sexual activity stems from a myriad of physiological, psychological, and interpersonal factors. Understanding the intricate mechanisms underlying this condition is essential for effective diagnosis, treatment, and support. In this blog, we will delve into the pathophysiology of painful intercourse, dissecting the neurological, hormonal, microbiological, psychological, and musculoskeletal components that contribute to its manifestation. By unravelling the scientific intricacies of this phenomenon, we aim to provide a comprehensive foundation for addressing the challenges faced by women experiencing painful intercourse.
Reasons for Pain
Painful intercourse, medically termed dyspareunia, encompasses a complex interplay of physiological, psychological, and interpersonal factors. At its core, the experience of pain during sexual activity is intricately tied to various mechanisms that warrant exploration. Neurologically, the vaginal and pelvic regions are densely populated with nociceptors which are specialized nerve endings that detect and transmit signals related to pain specialized sensory nerve endings. When stimulated by factors like friction, pressure, or inflammation, these nociceptors transmit pain signals to the brain via the spinal cord, contributing to the perception of pain during intercourse.
Hormonal balance, particularly governed by estrogen, is critical for maintaining vaginal health and lubrication. Fluctuations in estrogen levels, such as those occurring during menopause or due to hormonal contraceptives, can lead to vaginal dryness and thinning of vaginal tissues (atrophy), increasing susceptibility to pain during intercourse. Further, the delicate balance of the vaginal microbiota, comprising diverse bacteria and fungi, is vital for vaginal health and immune function. Disruptions in this balance, triggered by factors like antibiotics or hormonal changes, also can lead to opportunistic infections such as bacterial vaginosis or yeast infections, contributing to inflammation and discomfort during intercourse.
Also Read: PCOS: Infertility, Causes, Treatment & Lifestyle Modifications
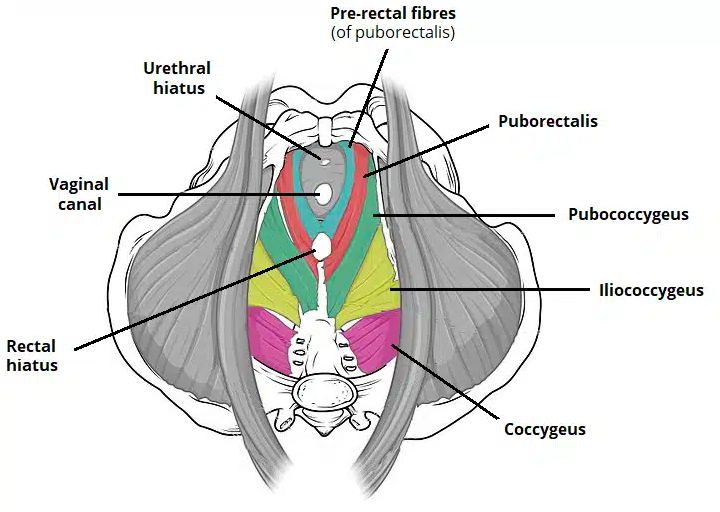
Psychological factors play a very important role in pain perception during intercourse. Anxiety, stress, depression, and past sexual trauma can heighten pain perception and disrupt arousal and lubrication. Addressing these psychological aspects is crucial for the holistic management of painful intercourse. The pelvic floor muscles, including the pubococcygeus, iliococcygeus, and puborectalis muscles, provide crucial support to pelvic organs and contribute to urinary and faecal continence and proper sexual function. Dysfunctions in these muscles, such as hypertonicity or weakness, also can manifest as pelvic pain and sexual dysfunction.
Painful Intercourse – Conditions
Dyspareunia
Dyspareunia, a condition characterized by persistent or recurrent pain during sexual intercourse, affects individuals of all ages and genders. It encompasses a spectrum of physical, psychological, and interpersonal factors contributing to discomfort or pain during sexual activity. Physically, dyspareunia may result from insufficient lubrication, vaginal infections, pelvic floor muscle disorders, hormonal imbalances, or structural abnormalities like endometriosis or vaginal atrophy. Psychological factors such as anxiety, stress, depression, past sexual trauma, or relationship issues can heighten pain perception and interfere with sexual arousal and lubrication, exacerbating the experience of dyspareunia.
The impact of dyspareunia extends beyond physical discomfort to encompass emotional distress and strained relationships. Individuals experiencing dyspareunia may feel frustrated, embarrassed, or inadequate, leading to anxiety about sexual performance and intimacy. Painful intercourse can strain communication between partners and undermine relationship satisfaction. Seeking timely medical evaluation and treatment is crucial for addressing dyspareunia and restoring sexual health and intimacy. Treatment options may include medical interventions to address underlying conditions, pelvic floor therapy, lifestyle modifications and psychological support. However, they can regain control over their sexual health and well-being, enhancing overall quality of life and relationship satisfaction with adequate and appropriate medical and lifestyle support.
Vaginismus
Vaginismus is a condition characterized by involuntary spasms of the pelvic floor muscles, particularly the pubococcygeus, iliococcygeus, and puborectalis muscles, in response to attempted penetration. Fear, anxiety, past trauma, or learned behaviours associated with penetration trigger these contractions, making penetration painful or impossible. This condition significantly impacts sexual health and relationships, leading to avoidance of sexual activity, frustration, and distress for both partners. Addressing underlying psychological factors and providing therapeutic interventions, such as pelvic floor physical therapy and relaxation techniques, is essential for managing vaginismus and restoring sexual function.
Vulvodynia
Vulvodynia refers to chronic pain or discomfort in the vulvar area, encompassing various types such as generalized vulvodynia and localized vulvodynia. Generalized vulvodynia involves pain experienced throughout the vulva, while localized vulvodynia affects specific areas like the vestibule or clitoris. Contributing factors to vulvodynia include hormonal changes, nerve irritation, muscle spasms, genetic predisposition, and past vaginal infections or trauma. Symptoms may include burning, stinging, or rawness in the vulvar area, heightened sensitivity to touch, and discomfort during sexual activity or prolonged sitting. Managing vulvodynia involves a multifaceted approach, including medical interventions to address underlying conditions, lifestyle modifications, and psychological support.
Treatment for Painful Intercourse
Medications are usually prescribed to manage underlying conditions that may be causing painful intercourse. For example, topical or oral medications may be used to treat vaginal infections, such as yeast infections or bacterial vaginosis, which can contribute to inflammation and discomfort during intercourse. Hormone therapy, such as estrogen replacement therapy or vaginal estrogen creams, may be prescribed to address hormonal imbalances associated with conditions like menopause or vaginal atrophy, improving vaginal lubrication and tissue health. Additionally, pain relievers or muscle relaxants may also be prescribed to alleviate pelvic pain or muscle tension, providing temporary relief during sexual activity.
In cases where structural abnormalities or anatomical issues are identified as the underlying cause of painful intercourse, surgical intervention may be recommended. For example, surgical procedures may be performed to remove endometrial implants or adhesions in individuals with endometriosis, reducing pain and improving sexual function. In cases of pelvic organ prolapse, where pelvic organs such as the uterus, bladder, or rectum descend into the vaginal canal, surgical repair may be necessary to restore pelvic floor support and alleviate discomfort during intercourse. Surgical interventions are typically considered after thorough evaluation and discussion with a healthcare provider to assess risks and benefits and determine the most appropriate treatment approach for the individual’s goals and needs. Counselling or psychotherapy also may be beneficial for addressing psychological factors contributing to painful intercourse, such as anxiety, stress, depression, or past trauma.
Lifestyle modifications and self-care practices can complement medical and therapeutic interventions in managing painful intercourse. Simple measures such as using water-based lubricants or vaginal moisturizers can improve vaginal lubrication and reduce friction during intercourse. Engaging in regular exercise, particularly activities that promote relaxation and stress reduction like yoga or meditation, can help alleviate muscle tension and enhance overall sexual health. Pelvic floor therapy, which involves exercises, biofeedback, manual techniques, and relaxation strategies to improve pelvic floor muscle function is also helpful to reduce pelvic pain and tension. Additionally, practising good hygiene, wearing comfortable clothing, and avoiding irritants like perfumed products or harsh soaps in the genital area can help maintain vulvar health and reduce discomfort.
How can we help?
At our practice, we understand the sensitive nature of sexual health concerns and offer comprehensive support to address them effectively. With gynaecologists, infertility specialists, and lifestyle experts on our panel, we provide a holistic approach that integrates medical management with lifestyle interventions. Our team collaborates to tailor treatment plans that encompass both medical interventions, such as medication and surgical procedures, and lifestyle modifications, including diet and exercise recommendations. By combining expertise in gynaecology, reproductive health, and lifestyle management, we aim to empower individuals to improve their sexual health and overall well-being. Contact us today to learn more about how we can support you on your journey towards a fulfilling and pain-free sexual experience.









1 comment
[…] Also Read: Painful Intercourse in Women – Reasons & Treatment […]