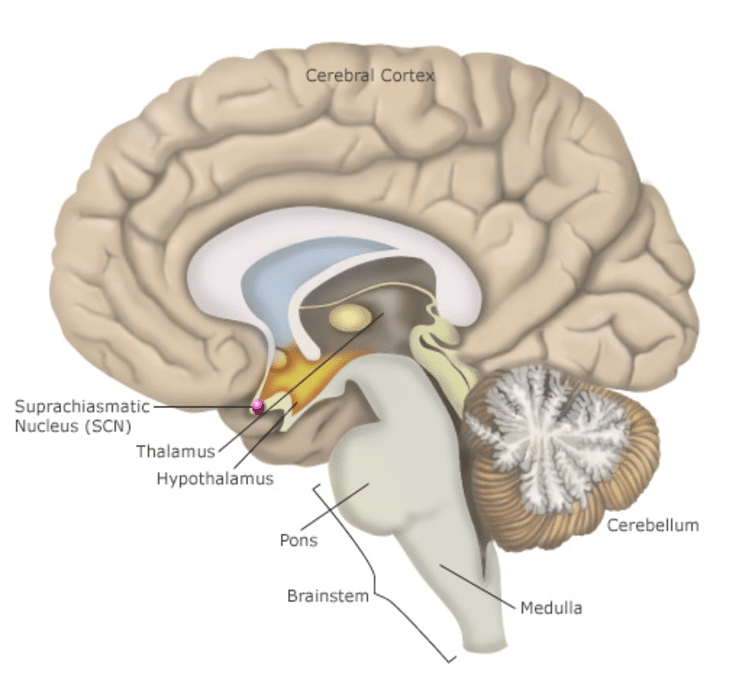
Circadian rhythms are 24-hour cycles that regulate various physiological processes in the body, including sleep-wake cycles, hormone release, body temperature, and metabolism. These rhythms are primarily driven by the body’s internal clock, located in the suprachiasmatic nucleus of our brain. But they are also influenced by external factors such as light, temperature, and social cues.
Circadian rhythm disorders occur when there is a misalignment between an individual’s internal body clock and the external environment. This can result in difficulties falling asleep, staying asleep, or waking up at appropriate times, leading to impaired daytime functioning.
Maintaining a healthy circadian rhythm is crucial for optimal physical and mental well-being. Disruptions to this have been associated with various health problems, including mood disorders, cognitive impairment, and metabolic disorders. It can even lead to an increased risk of chronic diseases such as diabetes and cardiovascular disease.
Also Read: Snoring & Sleep Apnea – Management Tips
Types of Circadian Rhythm Disorders
Circadian rhythm disorders encompass a range of conditions that disrupt the natural sleep-wake cycle. Understanding the distinct types of these disorders is essential for proper diagnosis and management. Here are the main types if circadian rhythm disorders:
Delayed Sleep Phase Disorder (DSPD): DSPD is characterized by a delayed onset of sleep compared to the typical bedtime. This causes individuals to have difficulty falling asleep until late at night or early morning hours. This delay can lead to difficulty waking up in the morning, resulting in daytime sleepiness and impaired functioning.
Advanced Sleep Phase Disorder (ASPD): ASPD is the opposite of DSPD. In APSD individuals experience an earlier-than-normal onset of sleep and wake up much earlier than desired. People with ASPD may find themselves falling asleep in the early evening and waking up very early in the morning. This pattern can disrupt social and occupational activities.
Non-24-Hour Sleep-Wake Disorder (Non-24). Non-24 is a condition where an individual’s internal body clock runs on a cycle longer than 24 hours. This leads to a gradual shift in sleep-wake times. This results in a pattern of sleep onset and wake times that drift later and later each day. Non-24 is commonly observed in blind individuals who lack the light perception to synchronize their internal clock with the external day-night cycle.
Shift Work Sleep Disorder (SWSD): SWSD occurs when individuals work non-traditional hours, such as night shifts or rotating shifts, disrupting their natural circadian rhythm. This can lead to difficulty sleeping during the day and staying awake or alert during work hours, resulting in impaired performance and an increased risk of accidents or errors.
Irregular Sleep-Wake Rhythm Disorder: This disorder is characterized by irregular sleep-wake patterns with fragmented sleep episodes occurring throughout the day and night. Individuals with irregular sleep-wake rhythm disorder may have difficulty maintaining a consistent sleep schedule, leading to excessive daytime sleepiness and impaired daytime functioning.
Also Read: Sleep Walking – Risks & Management Methods
Causes of Circadian Rhythm Disorders
Circadian rhythm disorders can arise from various factors, both internal and external, disrupting the body’s natural sleep-wake cycle. Here are the primary contributing factors for such disorders –
Biological factors: The body’s internal clock, located in the suprachiasmatic nucleus of the brain, plays a central role in regulating circadian rhythms. Disruptions to this biological clock, such as alterations in neurotransmitter signalling or changes in clock gene expression, can lead to circadian rhythm disorders. Additionally, age-related changes in circadian rhythm regulation may contribute to sleep disturbances, particularly in older adults.
Environmental factors: External cues, such as light exposure, temperature fluctuations, and social activities, synchronize the body’s internal clock with the external day-night cycle. However, exposure to artificial light at night, irregular sleep schedules, and shift work can disrupt this synchronization, leading to circadian rhythm disturbances. Travel across multiple time zones can also cause temporary circadian misalignment, commonly known as jet lag.
Genetic predisposition: Genetic factors can influence an individual’s susceptibility to circadian rhythm disorders. Variations in genes involved in circadian rhythm regulation, such as Period genes and Clock genes, can predispose individuals to sleep disturbances. Additionally, certain genetic conditions, such as familial advanced sleep phase syndrome, are associated with inherited alterations in circadian rhythm function.
Lifestyle factors: Poor sleep habits, such as irregular sleep schedules, excessive caffeine or alcohol consumption, and insufficient exposure to natural light during the day, can disrupt circadian rhythms and contribute to the development of sleep disorders. Stress, anxiety, and psychiatric conditions may also impact circadian rhythm regulation, exacerbating sleep disturbances.
Also Read: Narcolepsy – Tips to improve sleep
Symptoms & Diagnosis
Circadian rhythm disorders manifest through various symptoms that affect sleep quality and daytime functioning. Here are the common indicators and diagnostic approaches:
Common symptoms of circadian rhythm disorders:
- Difficulty falling asleep or staying asleep at desired times.
- Excessive daytime sleepiness or fatigue.
- Irregular sleep-wake patterns, such as waking up too early or too late.
- Difficulty concentrating or performing tasks during waking hours.
- Mood disturbances, including irritability, anxiety, or depression.
- Impaired social or occupational functioning due to sleep disturbances.
Diagnostic criteria and methods: Diagnosis of circadian rhythm disorders typically involves a thorough assessment of sleep patterns, medical history, and lifestyle factors. Healthcare providers may use various diagnostic tools and methods, including:
- Sleep logs or diaries to track sleep-wake patterns over several days or weeks.
- Actigraphy, a non-invasive method of monitoring sleep-wake cycles using wrist-worn devices that record movement patterns.
- Polysomnography (sleep study) to evaluate sleep architecture and identify any underlying sleep disorders, such as sleep apnea or restless legs syndrome.
- Questionnaires or standardized assessments to assess sleep quality, daytime functioning, and symptoms of circadian rhythm disruption.
Also Read: Restless Leg Syndrome
Management of Circadian Rhythm Disorders
Managing circadian rhythm disorders involves a combination of both medical interventions and lifestyle modifications.
In some cases, healthcare providers may prescribe medications to help regulate sleep-wake cycles and improve sleep quality. These medications may include melatonin supplements, sedatives, or wake-promoting agents.
Light therapy: Light therapy involves exposure to bright light, typically in the morning, to help reset the body’s internal clock and synchronize circadian rhythms. This therapy is particularly beneficial for individuals with delayed sleep phase disorder or seasonal affective disorder (SAD).
Chronotherapy: Chronotherapy involves gradually shifting sleep-wake times over days or weeks to adjust to desired schedules. This approach can be effective for individuals with delayed or advanced sleep phase disorder, as well as shift work sleep disorder.
Sleep hygiene practices: Implementing good sleep hygiene habits, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment (e.g., comfortable mattress, dark room), can promote better sleep quality and help regulate circadian rhythms.
Regular exercise: Engaging in regular physical activity, particularly during the daytime, can promote better sleep quality and overall health. However, it is essential to avoid vigorous exercise close to bedtime, as it may interfere with sleep initiation.
Exposure to natural light: Spending time outdoors during daylight hours and ensuring adequate exposure to natural light can regulate circadian rhythms and promote wakefulness during the day. Conversely, limiting exposure to artificial light, especially in the evening, can signal the body to prepare for sleep.
Stress management: Practicing relaxation techniques, such as deep breathing exercises, meditation, or yoga, can reduce stress levels and promote better sleep. Managing stress effectively can also mitigate the impact of circadian rhythm disorders on overall well-being.
Also Read: Insomnia – Management Strategies
How can we help?
At SOLVEMyHealth, our multidisciplinary team is dedicated to providing comprehensive support for individuals struggling with circadian rhythm disorders. Our doctors specialize in sleep medicine, offering expert diagnosis and personalized treatment plans tailored to your specific needs. Our psychologists provide emotional support and cognitive-behavioural techniques to address any underlying stress or anxiety contributing to sleep disturbances. Additionally, our lifestyle experts in diet and exercise offer guidance on optimizing your daily routines to promote better sleep health. We empower you with the tools and resources needed to overcome circadian rhythm challenges to improve sleep