Parasomnias are a spectrum of sleep disorders characterized by abnormal behaviours, movements, emotions, perceptions, or dreams during sleep. Unlike disturbances that affect sleep quality or timing, parasomnias involve peculiar experiences or activities during various sleep stages. These experiences range from benign phenomena like sleep talking to more disruptive actions such as sleepwalking or vivid dream enactments. Parasomnias can manifest during different sleep stages, including non-rapid eye movement (NREM) and rapid eye movement (REM) sleep, each exhibiting distinct characteristics.
Historically, the study of parasomnias traces back to ancient times, with early mentions found in religious texts and medical writings. Modern scientific understanding has significantly advanced, with developments in sleep medicine and neurology. Pioneering research in the 20th century, particularly in polysomnography, has improved the ability to diagnose and categorize parasomnias accurately. Despite this progress, misconceptions and stigmas surrounding parasomnias persist, emphasizing the need for increased awareness and education about these disorders.
The prevalence and incidence of parasomnias vary, with certain types being more prevalent in specific age groups. Epidemiological studies suggest that childhood parasomnias like sleepwalking and sleep talking are relatively common, while disorders such as REM sleep behaviour disorder are more frequently observed in older adults. Estimating precise prevalence rates remains challenging due to underreporting, misdiagnosis, and cultural variations in sleep-related behaviours.
Also Read: Restless Leg Syndrome & its impact on sleep
Types of Parasomnias
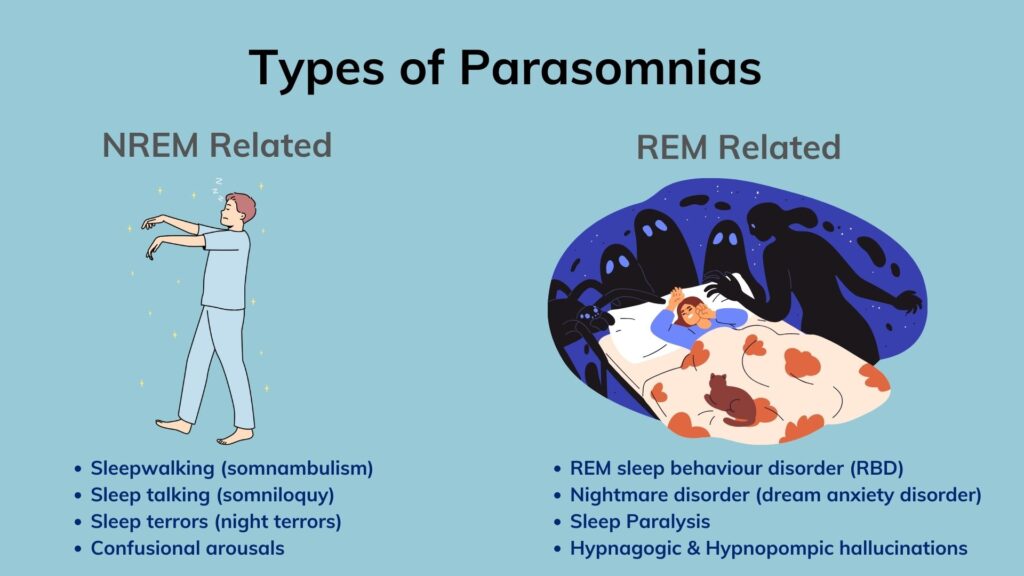
As discussed, parasomnia encompasses a diverse range of sleep disorders, each presenting unique characteristics and behaviours. These disorders are broadly categorized into two main types –
- Non-Rapid Eye Movement (NREM) Parasomnias and
- Rapid Eye Movement (REM) Parasomnias.
Non-Rapid Eye Movement (NREM) Parasomnia
NREM Parasomnias involve abnormal behaviours or experiences during non-rapid eye movement sleep stages. This usually occurs during the first half of the night. These include sleepwalking (somnambulism), sleep talking (somniloquy), sleep terrors (night terrors), and confusional arousals. Sleepwalking involves engaging in activities such as walking or performing complex behaviours while still asleep, often with no recollection of all these upon waking up. Sleep talking involves vocalizing during sleep, ranging from simple sounds to coherent speech. Sleep terrors are characterized by sudden episodes of intense fear or panic during sleep, often accompanied by screaming, rapid heart rate, and sweating. Confusional arousals involve periods of disorientation or confusion upon awakening from sleep, often accompanied by behaviours such as sitting up, thrashing, or mumbling.
Rapid Eye Movement (REM) Parasomnia
On the other hand, REM Parasomnias occur during the rapid eye movement (REM) sleep stage. This is often associated with vivid dreaming. These disorders include REM sleep behaviour disorder (RBD), nightmare disorder (dream anxiety disorder), sleep paralysis, and hypnagogic and hypnopompic hallucinations. RBD involves acting out dreams during REM sleep, leading to potentially dangerous behaviours such as punching, kicking, or yelling. Nightmare disorder involves recurrent nightmares that cause distress or impairment in daily functioning. Sleep paralysis is characterized by temporary paralysis upon awakening or falling asleep, often accompanied by hallucinations or a sense of impending danger. Hypnagogic hallucinations occur as individuals fall asleep, while hypnopompic hallucinations occur upon waking, involving vivid sensory experiences that may feel real but are not.
Parasomnia – Causes and Risk Factors
Parasomnias stem from a combination of biological, environmental, and psychological factors. These factors can contribute to disruptions in the normal sleep cycle, leading to parasomnias.
Biological factors play a significant role in the development of parasomnias. Genetics can predispose individuals to certain parasomnias, as they may inherit genetic variations that affect sleep regulation and arousal mechanisms. Neurological abnormalities, such as dysfunction in the brain regions responsible for sleep-wake transitions, can also contribute to parasomnias. Additionally, imbalances in neurotransmitters, such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), also may disrupt sleep processes and increase the risk of parasomnias.
Environmental factors can also influence the occurrence of parasomnias. Stress and anxiety can disrupt sleep patterns and trigger episodes of parasomnia. Substance abuse, including alcohol, caffeine, and certain medications, can alter brain chemistry and interfere with sleep regulation, potentially exacerbating parasomnias. Medications, such as antidepressants, stimulants, and sedatives, may also have side effects that contribute to parasomnias.
Also Read: Narcolepsy – Treatment & Management Strategies
Other contributing factors include sleep deprivation, irregular sleep schedules, and underlying medical conditions such as sleep disorders, neurological disorders, or psychiatric disorders. Certain lifestyle habits, such as excessive screen time before bed, poor sleep hygiene practices, or sleeping in an unfamiliar environment, can also increase the risk of parasomnias.
Parasomnia – Diagnosis
Diagnosing parasomnias involves a combination of clinical assessment and specialized sleep studies. Clinical assessment typically begins with a thorough medical history and evaluation of symptoms. It may involve detailed descriptions of sleep-related behaviours and experiences provided by the patient or their bed partner. Your doctor may also inquire about family history, medications and lifestyle factors. He may also enquire about other underlying medical or psychiatric conditions that could contribute to parasomnias.
In addition to clinical assessment, specialized sleep studies, such as polysomnography, are often used to diagnose parasomnias. Polysomnography involves monitoring various physiological parameters during sleep, including brain activity, eye movements, muscle tone, heart rate, and breathing patterns. This comprehensive evaluation helps identify abnormalities in sleep architecture and patterns associated with specific parasomnias.
Differential diagnosis is essential to distinguish parasomnias from other sleep disorders or medical conditions that may present with similar symptoms. Certain other conditions such as sleep-related epilepsy, nocturnal seizures, nocturnal panic attacks, and psychiatric disorders can mimic parasomnias. Hence it requires careful evaluation to ensure accurate diagnosis and appropriate treatment.
Also Read: Restless Leg Syndrome & its impact on sleep
Management Strategies for Parasomnia
Managing parasomnias involves a multifaceted approach that involves medical interventions, lifestyle modifications, and environmental adjustments tailored to each patient.
Medical interventions may include pharmacotherapy, which involves medications to target specific symptoms or underlying causes of parasomnias. For example, medications such as benzodiazepines or antidepressants may be prescribed to reduce arousal levels, manage anxiety, or improve sleep quality. However, it’s essential to weigh the potential benefits vs risks of medication therapy and monitor for any adverse effects.
Cognitive-behavioural therapy (CBT) is another effective approach for managing parasomnias. CBT aims to identify and modify maladaptive thoughts, behaviours, and sleep patterns that contribute to parasomnias. Techniques such as relaxation training, sleep hygiene education, and stimulus control can help improve sleep quality and reduce the frequency and severity of parasomnic episodes.
In addition to medical and psychological interventions, lifestyle modifications play a crucial role in managing parasomnias. Adopting good sleep hygiene practices, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment, can promote better sleep quality and reduce the likelihood of parasomnic events.
Environmental adjustments, such as implementing safety precautions in the bedroom to prevent injury during sleepwalking episodes or minimizing potential triggers for nightmares, are also important components of managing parasomnias. For example, removing obstacles or hazards from the bedroom, installing safety gates or locks, and using nightlights or white noise machines can help create a safe and conducive sleep environment.
How can we help you?
At SOLVEMyHealth, we understand the challenges that individuals facing parasomnias encounter and are dedicated to providing comprehensive support and solutions to help you manage your condition effectively. With our online doctor consultations, you can connect with experienced healthcare professionals from the comfort of your home. For those who require further evaluation, our home sleep study facility offers a convenient and non-invasive way to monitor sleep patterns. Our team is well-versed in diagnosing and treating parasomnias, and they will work closely with you to develop personalized treatment plans tailored to your unique needs and preferences.
In addition to medical interventions, our platform offers access to psychologists who specialise in cognitive-behavioral therapy (CBT). CBT is highly effective in managing parasomnias by addressing underlying thoughts, behaviours, and sleep patterns that contribute to the condition. Our team will guide you through evidence-based techniques and strategies to help improve your sleep quality and reduce the frequency and severity of parasomnic episodes.
Furthermore, our lifestyle experts are available to provide support and guidance on adopting healthy lifestyle habits that can complement your treatment plan. Whether it’s optimizing your diet, incorporating regular exercise into your routine, or implementing stress management techniques, our team will empower you to make positive changes that promote better sleep and overall well-being.